Restore Your Heart’s Potential with Coronary Stents.
All About Heart Stents
How are Coronary Artery Stents Deployed?
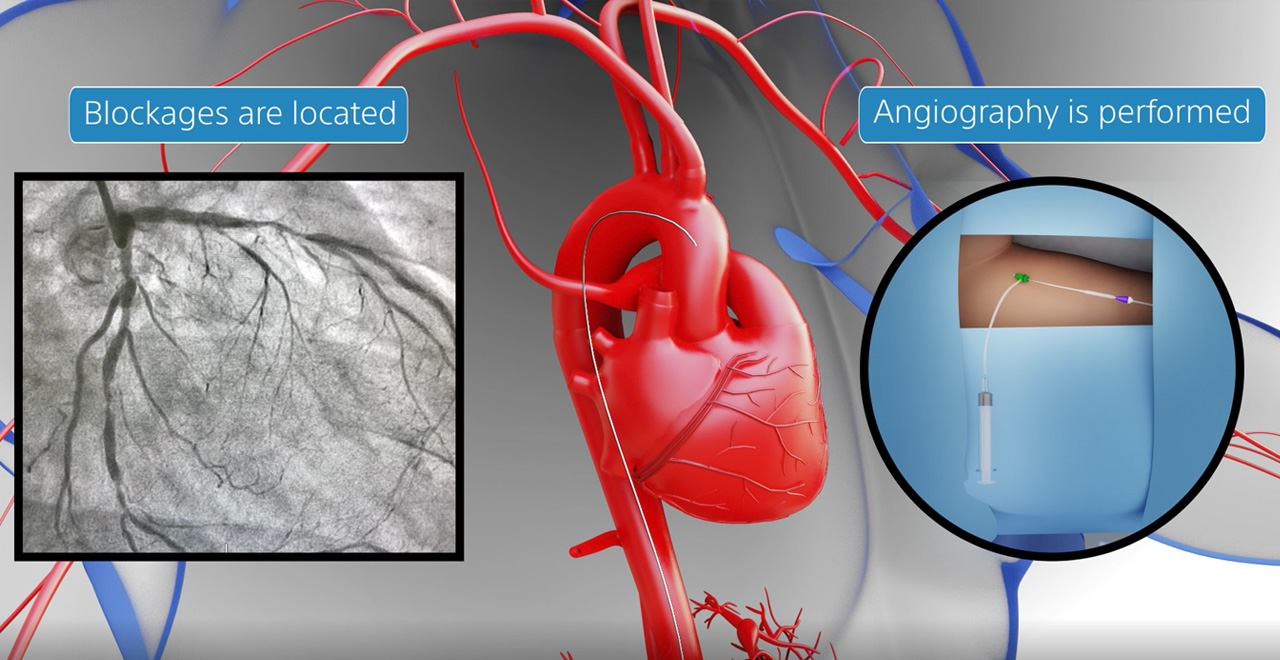
The patient is given a local anesthetic with a small incision in the groin/wrist to access the artery. A thin, flexible catheter tube is inserted through the incision and guided up to the blocked or narrowed artery using X-ray guidance. A small balloon at one end of the catheter is inflated to widen the artery, and the stent is then placed over the balloon and expanded inside the artery.
Once the stent gets placed at the specified point, the balloon gets deflated and removed, leaving the stent to hold the artery open. The medication coating on the stent begins to release slowly over time, helping to prevent scar tissue from forming inside the stent and reducing the risk of re-narrowing.
The patients are monitored in the hospital post-procedure for a short time to ensure no complications. They may need medications to prevent blood clots and help the artery heal properly. Patients do return to their normal activities within a week after the procedure.
Different Types of Coronary Stents and Their Functions
Bare-Metal Stents
Bare-metal stents are the oldest type of coronary stents and consist of a wire mesh tube placed in the blocked artery. These stents have been used for decades and are known for their durability and strength. However, they have a higher rate of renarrowing, which may require repeat procedures.
Drug-Eluting Stents
Drug-eluting stents coated with medications help prevent the artery from re-narrowing after the stent is placed. These stents are the most used type of coronary stent today. The medicines used on the stent are slowly released over time, which helps to prevent the formation of scar tissue inside the stent.
Frequently Asked Questions
What is a coronary stent, and how does it work?
A coronary stent is a small, metal mesh tube placed inside a narrowed or blocked coronary artery to improve blood flow to the heart muscle. It supports the artery walls and prevents them from collapsing or narrowing again.
What is the difference between a bare-metal stent and a drug-eluting stent?
A bare-metal stent is a coronary stent made of metal containing no medication. A drug-eluting stent, on the other hand, has a coating that releases medication slowly over time to help prevent the artery from becoming narrow again.
Who needs a coronary stent?
Coronary stents are typically recommended for patients with coronary artery disease who have significant blockages in their arteries that are causing chest pain or other symptoms. They may also be used in emergency situations, such as during a heart attack, to restore blood flow to the heart muscle quickly.
What are the benefits of a drug-eluting coronary stent?
The main benefit of a drug-eluting coronary stent is a lower risk of re-narrowing the artery compared to bare-metal stents. This is because the medication coating helps avoid scar tissue formation inside the stent. Drug-eluting stents also have a lower risk of heart attack.
How is a coronary stent placed in the artery?
A coronary stent is typically placed during a procedure called a coronary angioplasty. A small incision is done in the groin or wrist, and a thin tube called a catheter is inserted through the incision and guided up to the blocked or narrowed artery using X-ray guidance. A small balloon at one end of the catheter is inflated to widen the artery, and the stent is then placed over the balloon and expanded inside the artery.
Are there risks associated with getting a coronary stent?
Similar to any medical procedure, getting a coronary stent is associated with risks. These can include bleeding, infection, allergic reactions to medication, damage to the artery or other organs, and blood clots. However, the risk of complications are pretty minimal, and the benefits of the procedure take away the risk if it is done successfully.
How long does it take to recover after getting a coronary stent?
Most patients go back to their normal activities in a week or so after getting a coronary stent. However, it is essential to follow the instructions given by your heart specialist for post-procedure care, which includes taking medications to prevent blood clots and avoiding strenuous activity for a specific time period.
Subscribe to Platinum For Heart Newsletter
Sign up now and get free access to our monthly newsletter on Heart health & More
Disclaimer: The information presented by Boston Scientific Corporation is for educational purposes only and does not recommend self-management of health issues. The information should not be treated as comprehensive and does not intend to provide diagnosis, treatment or any medical advice. Individual results may vary and hence, it is advisable to consult your doctor regarding any medical or health related diagnosis or treatment options.
IC-1625802AB-0623